This article, written by Penn State biologist and entomologist Andrew Read, originally appeared in the Centre Daily Times (CDT) on 29 April 2012. It was the first article in the bimonthly "Focus on Research" column, which highlights different research projects being conducted at Penn State.
As mosquitoes become more resistant to insecticides, Read and Thomas are working to develop a fungus to kill mosquitoes in an effort to contain the spread of malaria among humans. Credit: Hugh Sturrock
Evolution kills.
Last year, about 100,000 Americans died of infections that were easily curable 20 years ago, according to the Infectious Diseases Society of America. That’s more than twice the number of people the Insurance Institute for Highway Safety said were killed in car crashes. The cures are failing because germs are evolving. Nowadays, pathogens can evolve around drugs faster than replacement drugs can pass through regulatory hurdles. In a few cases, resistance has evolved so far that some germs can be killed only with chemicals that also kill the patient.
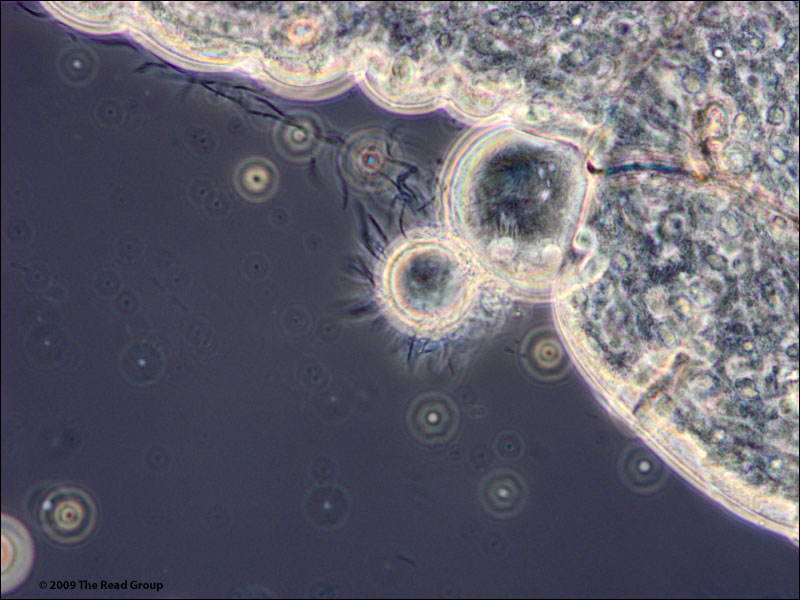
The microscopic images above (taken with an electron microscope) show bags of malaria parasites inside a mosquito. Each bag contains between 5,000 and 20,000 parasites. Andrew Read, director of the Center for Infectious Disease Dynamics at Penn State, and Matthew Thomas, a professor of entomology, are working to develop a fungus to kill mosquitoes, which are becoming resistant to insecticides. Credit: John Findlay, University of Edinburgh, Scotland.
In essence, the bugs are not taking our drugs lying down. Biologists call this incredible capacity of life to overcome environmental insults “adaptive evolution.” One of the key medical and scientific challenges in the 21st century is to discover how to manage the adaptive evolution of the pathogens we target with our pharmaceuticals. As an evolutionary biologist, I increasingly wonder whether misunderstandings of how adaptive evolution works are obscuring other strategies that might help our medicines perform better.
One thing we have learned is that a pathogen with a new genetic mutation that makes it resistant to a drug generally dies out if the patient is not treated with that drug. On the other hand, if there is aggressive drug treatment, the drug-resistant pathogen can erupt with a population explosion after our medicines have wiped out all the drug-sensitive pathogens. With the competition wiped out, the offspring of the new drug-resistant pathogen are free to multiply, becoming more abundant in the patient and increasing the likelihood of transmitting drug resistance to other patients. That is how MRSA evolved and became so prevalent in hospitals during the past decade.
Consider the current dogma that, to prevent drug resistance, it is essential that patients complete their drug courses even after they feel better. While it is true that dead pathogens can’t mutate to resistance, it also is true that aggressive pharmaceutical therapy can promote the very evolution it is intended to retard because it ensures that the resistant parasites that are present have the maximum evolutionary advantage.
My feeling is that the current thinking about resistance management focuses too much on preventing mutations and not enough on limiting their spread. Research at Penn State and elsewhere is striving to discover treatment strategies that do not strengthen the evolutionary advantage for any drug-resistant mutants that may evolve.
The microscopic images above (taken with an electron microscope) show bags of malaria parasites inside a mosquito. Each bag contains between 5,000 and 20,000 parasites. Andrew Read, director of the Center for Infectious Disease Dynamics at Penn State, and Matthew Thomas, a professor of entomology, are working to develop a fungus to kill mosquitoes, which are becoming resistant to insecticides. Credit: Krijn Paaijmans, Penn State University.
Ongoing work on malaria in my research group, funded by the National Institutes of Health, is aimed at identifying the best drug-treatment plan. We are trying a variety of regimens in mice, including reduced doses or intermittent treatment (once a week instead of every day, for example). All the regimens we have tried so far do better than standard practice at slowing the spread of resistance, and several do as well or even better at improving health and reducing infectiousness.
We may not need to use our chemicals to kill every parasite in order to achieve health while also helping our medicines win the evolutionary battle against drug-resistant pathogens. If there is a simple rule for managing the evolution of resistance, it is “impose no more selection than is absolutely necessary for patient health.” Often the immune system just needs a helping hand — and immunity can be a lethal weapon against drug-resistant parasites.
I think we do not yet have adequate knowledge to decide, for any infectious disease, the best way to treat patients with pharmaceuticals for infectious diseases. So for the time being, everyone should stick with current practice. But I think our work illustrates the need for a rigorous, evidence-based science of adaptive evolution in the medical context. Researchers in this field hope to discover the optimum treatment regimens that deliver the health that physicians and their patients want while mitigating, as much as possible, the evolution of drug-resistant pathogens.
Drug-use policies represent humankind’s greatest attempt to deliberately shape the future evolution of any organisms. We need evolutionary science to do it right.
Andrew Read is the director of the Center for Infectious Disease Dynamics at Penn State.